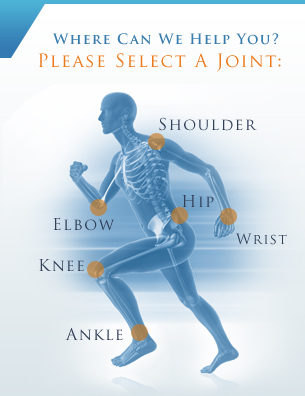
Procedures: Shoulder
|
|
Arthroscopic Rotator Cuff Repair
 The rotator cuff is a group of tendons and muscles that support the shoulder joint and allow for complete movement while keeping the ball of the arm bone in the shoulder socket. These tendons and muscles may become torn or otherwise damaged from injury or overuse and can lead to pain, weakness and inflammation. Surgery may be used to treat this often serious condition.
The rotator cuff is a group of tendons and muscles that support the shoulder joint and allow for complete movement while keeping the ball of the arm bone in the shoulder socket. These tendons and muscles may become torn or otherwise damaged from injury or overuse and can lead to pain, weakness and inflammation. Surgery may be used to treat this often serious condition.
Rotator cuff repair is performed under general anesthesia and aims to reattach the tendon back to the arm, along with removing any loose fragments from the shoulder area. Most rotator cuff procedures can now be performed through arthroscopy, which uses a few tiny incisions rather than one large incision. This technique offers patients minimal trauma, less scarring and less damage to surrounding tissue.
Rotator cuff repair surgery is usually successful in relieving shoulder pain, although full strength cannot always be restored. Patients must undergo physical therapy after surgery, and it may take months for the shoulder to fully heal. Arthroscopic rotator cuff repair is considered much safer than the traditional procedure, although risks such as infection, pain or stiffness, nerve damage or the need for repeated surgery do still exist. These risks are considered rare, as most people achieve successful outcomes from this procedure.
Broken Collarbone (Clavicle Fracture) Treatment
The clavicle, commonly known as the collarbone, is the bone of the shoulder joint that connects the arm to the rest of the body. Clavicle fractures most frequently occur as a result of trauma from a blow to the shoulder, fall or motor vehicle accident. They are most common in young children and older adults who are more susceptible to fractures.
Clavicle fractures cause the shoulder to slump downward and a bruise to appear over the fractured area. Some patients may hear a snapping sound when the fracture occurs. Pain is often experienced at the time of fracture and when the area is touched. Patients may also experience pain while trying to move the arm.
If you experience a collarbone fracture, you should seek immediate medical attention. Your doctor will take a brief medical history and examine your shoulder to determine whether or not a fracture has occurred. X-rays may be taken to determine the type and severity of the fracture.
Many fractured collarbones can be treated at home through conservative methods such as immobilization, aspirin, ibuprofen and a sling. Your doctor may instruct you to wear a sling at all times until pain subsides, which can take two to eight weeks depending on your age and the severity of your fracture. Patients whose bone has moved after the fracture may require surgery to repair the bone and allow it to heal properly.
Frozen Shoulder (Adhesive Capsulitis) Treatment
Frozen shoulder, also known as adhesive capsulitis, is a common condition that causes pain and stiffness in the shoulder as a result of a tightening or thickening of the capsule that protects the structures of the shoulder. Although the specific cause of this condition is not known, it most often occurs after recent immobilization of the joint or as a complication of diabetes. Frozen shoulder most often affects patients between the ages of 40 and 60.
Patients with frozen shoulder often experience pain, stiffness and limited range of motion that gradually worsens as the joint becomes more and more frozen. Eventually, the shoulder will shift into its thawing phase, during which pain and stiffness subside and range of motion is slowly restored.
Your doctor can diagnose frozen shoulder after a thorough evaluation of your condition, as well as an X-ray or MRI examination, which helps rule out other possible shoulder conditions.
Treatment for frozen shoulder usually focuses on managing pain and other symptoms as the condition progresses. This may include anti-inflammatory medications, corticosteroids and physical therapy. Minimally invasive surgical procedures, such as distension, arthroscopy and manipulation, may also be performed with a goal of stretching or releasing the contracted joint capsule.
« Previous 1 2 3 4 Next »